After I married my husband, I often imagined what our future would be like together. I pictured what our home life would be like. A steady stream of chaos with kids going to and fro, countless activities, gadgets littered about the yard, leaving no question to onlookers that kids were being raised there. I thought of what my husband would be like as a father. The laughter of a young girl held high as they splashed about the water; the tears of a toddler wiped away as he healed scraped knees with a gentle kiss; the excitement of a baseball capped boy as they embarked on a path– fishing rods slung over their shoulders and finally, the scowl of a teen who just can’t handle being beat by Dad at a game of hoops.
Dreams of a big family were becoming a reality when, in early July, we discovered we were expecting Baby #2. Our daughter was 15 months old at the time, and we were absolutely ecstatic (and mildly worried) to know that our children would be just two years apart. There I was, imagining the future again, already envisioning what their relationship would be like. Soft giggles, squeals of delight, secrets whispered into tiny ears and even the shouts of a play session gone wrong. I knew they would be playmates, best friends, and confidantes. And I could not wait for it all to happen.
I was looking forward to being pregnant again. My first was a textbook pregnancy. I simply did what the doctor told me to do and waited patiently for baby’s birth day. I went for the requisitioned ultrasounds, drank the sugary drink and planned a hospital birth. It was, after all, my first pregnancy and this is what pregnant women did, right? I was naïve.
Without the slightest blink of an eye, my husband and I went for our 12-week ultrasound (also known as a nuchal translucency). We marvelled at the sight of our first baby, left the clinic with a CD of images we couldn’t wait to share and a report, which found its way to the depths of my purse never to be seen again.
Fast forward to pregnancy number two. This time around, I was a little more versed in the realm of pregnancy. I knew that there was such a thing as prenatal testing that I did not have to have my baby in the hospital, and that there was such a thing as a doula. This time, I knew that a nuchal translucency was used to test for chromosomal abnormalities. I didn’t care about that. Didn’t think anything like that would ever happen to me anyway. Didn’t have the “what if” conversation with my husband. Only knew that I wanted to see my baby. And I did.
12 weeks gestation: Baby is just a tiny little bean bouncing all over the place but already, we see limbs, a spine and nubby fingers and toes. I am completely mesmerized by the sight of this life growing inside me as the sonographer takes measurements in order to satisfy the requirements of the test. We are giddy with excitement over the sight of our baby; trying to wage guesses as to baby’s gender. The giddiness dissipates quickly. The doctor comes in to deliver the news that there is a chance the baby I am carrying has Down syndrome – a one in 11 chance to be exact. Odds I will NEVER forget.
The doctor talked to us briefly about Down syndrome and what it could potentially mean for our baby. Our child would be developmentally delayed. Our child may face additional health problems such as a heart condition, which may require major surgery. If the doctors knew of any potential complications in advance, they could prepare for them and provide ongoing monitoring and care throughout my pregnancy. We could pursue further testing. We could wait and see. We could terminate. I was immediately transported to my baby’s birth day, imagining those first few moments with my baby. Then being slapped with the news our baby had Down syndrome, our baby would not be coming home with us and would need a major surgery right away. How would I handle that? Who would care for our daughter? I panicked at all the “what ifs” but tried to remain optimistic that everything would be fine. It was a quiet drive home.
My husband and I had to ask ourselves some pretty tough questions. Testing came with risk. Unless we chose an amniocentesis, it was not completely accurate. I was afraid to wait and see. I wanted to be prepared. Termination was off the table. We knew that without ever having had the “what if” conversation. We had seen our baby already, seemingly already formed, and we were in love. True to our characters, we remained calm as we sifted through the sea of information, weighed the pros and cons and ultimately decided to pursue amniocentesis. If our baby did have Down syndrome, we wanted him/her to have the best possible care right out of the gate. More importantly, we wanted to be able to celebrate, rather than grieve our baby’s arrival, to be emotionally available to him/her and be in a stage of acceptance. We would use the remainder of my pregnancy to learn all we could about local resources, but I also knew that Down syndrome might be all I would think about for the next few months, overshadowing every other aspect of my pregnancy.
15 weeks gestation – September 16th, 2009: I am lying on the crinkly paper and trying not to even breathe as the doctor inserts a long needle. I watch my baby intently on the TV screen and pray my baby does not move during the 30 seconds the needle takes to fight its way through layers of skin and muscle. As soon as the doctor withdraws the needle, I turn to my husband and say: “I should not have done that.” I instinctively knew in three weeks I would get the call. I would get the call saying our baby had Down syndrome and there would be no more optimism, no more hoping. It would just be. And I would have to live out the remainder of my pregnancy with Down syndrome occupying each and every nook and cranny of my mind.
5 days later — September 22nd, 2009: I am sitting at my desk at work. My husband calls to say the clinic has left a message at the house for me to call them back. We were not expecting results for at least another two weeks so I wonder what the reason for the call was. My initial thought is that the test is inconclusive; that they are calling to tell me I have to schedule a second test. I quickly call the clinic, completely oblivious that the reason for the call might be to deliver the results. I am given the results, right there at work, over the phone. I hear the words: “Well, we have a problem. All of the cells we looked at show an extra chromosome which is indicative of Trisomy 21.” I am speechless yet search for words. The dead air is uncomfortable but I have no idea what to say. Finally, even though my husband and I had decided not to find out, I manage to muster, “Can you tell me the baby’s sex?” We are having a boy. The boy my husband so desperately wanted. The boy who would make us the million dollar family. The boy who has Down syndrome. It is the most bittersweet moment of my life. The doctor goes on to present our options; we can either choose to continue or terminate our pregnancy. It is an extremely accurate test. So accurate, in fact, that there is no chance that our reality will be anything else. We’d have the full report within a week. I hang up the phone, stare blankly into my computer screen, and wonder how to break the news to my husband.
The tears came hard and fast. I couldn’t control them and for two entire days I sobbed. And then, I cried harder because I was crying in the first place. I had just begun to feel my baby move and could not help but feel guilty for grieving this beautiful life growing inside of me. I knew I loved my baby and I could not comprehend why I was so upset. It was irrational and completely illogical. I had been mentally preparing myself that our baby having Down syndrome was a real possibility ever since we were given our risk assessment. But nothing could prepare me for the actual diagnosis. I was devastated. My husband said something to me, I will never forget. He said, “He is my son. I love him no matter what and I can’t wait to take him fishing.” I was so thankful he felt the same love I felt and that his dreams of fishing trips with his son didn’t change because of Down syndrome. Even with a supportive husband by my side, I was still crying and needed someone to help me understand why. We immediately met with a geneticist and he told me it was okay to grieve. It was okay to be upset about losing what you thought was coming – and that’s what it was – those visions of my children whispering and giggling, playing and confiding, quickly turned into visions of them not being able to communicate with one another, let alone play with each other. It was the geneticist who also put it all in perspective. Down syndrome did not mean my child couldn’t do things; it just meant he might take a little longer getting there. The important thing to remember, he said, is your baby is a baby first and will have needs just like your firstborn. He will develop on his own schedule just like any other child. He may (or may not) face additional health concerns but these are concerns that many children will face, regardless of whether they have Down syndrome or not. We left our meeting breathing a little easier and discovered there was a community rich in resources and support waiting for us to knock at the door.
18 weeks gestation: Our son looks like a baby now, more so than a bean. He is pretty active and definitely not shy; there is no denying he is a boy. He measures right on track, and to our surprise, the sonographer does not find one single genetic marker for Down syndrome. I am thinking, had we not done the amniocentesis, he looks to be more of the ten in 11, instead of the one in 11 odds. But, of course, we know he is the one in 11.
22 weeks gestation: I find myself once again under a paper sheet and a thick coat of gel. The wand smoothly glides over my round belly in search of baby’s heart during a fetal echocardiogram. I don’t see much else of my baby this time. So far, they tell me, his heart looks great.
Our baby’s development and growth were closely monitored. If our baby failed to continue to thrive, I would head straight for delivery. Even if baby did continue to thrive, I would be scheduled for induction between weeks 38 and 39. To go beyond week 39 was to risk stillbirth and we certainly did not want that. I was afraid of an induction. I had heard they sometimes lead to a caesarean section and I wanted to avoid that if at all possible. I didn’t want the added stress of having to recover from major surgery on top of everything else.
28 weeks gestation: The sonographer is kind of quiet. Something has changed. She leaves the room (never a good sign), and comes back to suggest I book a second fetal echocardiogram for the simple reason that our baby is more developed and it will be a good opportunity to get a really good look at everything. I know something is up.
32 weeks gestation: The doctor detects an abnormality with our baby’s heart. He has a dilated chamber, which, unbeknownst to me, the sonographer had spotted four weeks earlier. The real reason for this second fetal echocardiogram. It is a lengthy test; nearly three hours, and ultimately it’s too difficult to determine the cause of the dilation. The doctor presents us with a best/worst case scenario based on all probabilities. Baby’s heart will either correct itself or require a major surgery in Edmonton. I take the news surprisingly well. While I had hopes that this would not be, I know it is a possibility. It is the first time we are told not all is hunky dory and I worry about our baby’s future.
With an induction looming and a possible heart surgery for baby, I decide it is time to make my intention to breastfeed my son known to ALL doctors involved. It is important to me, no matter what the circumstances of his birth, that I be given time to bond with my child before he is whisked away to NICU (should that be where he ends up). His cardiologist immediately drafts a letter to the Labour and Delivery ward explaining that our baby’s heart condition is not immediately life threatening and there is no reason I should not be given the opportunity to bond and attempt breastfeeding after his birth.
Towards the end of my pregnancy, I felt I was at peace with our baby’s diagnosis and I was excited to meet him, just as any mother would be. My husband became so comfortable with the fact our baby had Down syndrome that, at one point, he told me he’d be upset if he didn’t. The nursery was ready, the baby clothes washed and tucked away neatly into drawers, the suitcase packed and ready by the door. But nothing could have prepared me for the morning of February 20th, 2010.
38 weeks gestation –February 19th, 2010: I am getting ready for an adventure with my almost-2-year-old daughter today – we are taking her first bus ride downtown to have lunch with Daddy. As we are on our way out the door, the phone rings. It is the hospital calling. They tell me to enjoy my weekend; they are too busy and won’t be calling me until at least Monday for an induction. As luck would have it, baby has his own plans.
6pm: We are just sitting down for supper and I am pretty sure my contractions have started. They are pretty mild so I am not really sure if this is it yet.
10pm: This is definitely it. I’ve been leaking small amounts of fluid for a while now. We aren’t in active labour enough to go into the hospital but we go anyway to determine whether the fluid is amniotic or not.
1:30am: The fluid is not amniotic so we are sent home to continue labouring, but not before I am given a shot of pain medication to help manage my intensifying contractions. I am told it will wear off in four hours and I will definitely be back once it does.
February 20th, 2010, 5am: I am waking up and I am starting to feel the contractions again but they are relatively mild so I lie in bed until nearly 6am. My husband is getting things together; we are taking our time, waiting for the contractions to get really intense before we head to the hospital.
6:15am: I get in the shower and all of a sudden, the contractions have me down on all fours. Every time I try to stand, I am floored with another. They are coming hard and fast and I can’t get enough of a break between them to stand up and move towards the car. I make my way into the bedroom, but there is still not enough of a break in between the contractions to get down the stairs and out the door. My husband is trying to help me but he is no match for the intensity of a contraction. He finally asks me if he should call 911. I tell him no, that I can do it, that I can get to the car. He asks again and I finally concede. While he is on the phone with the 911 dispatcher, my body bears down and I know we are in trouble. This baby is coming and he is coming NOW.
7:01am: The Calgary Fire Department arrives on scene. I think they think they’re going to pack me into an ambulance and send me on my way but the next contraction proves otherwise. Baby is crowning.
7:04 am: EMS arrives on scene. My body bears down one more time and I feel our baby coming.
7:09 am: A second EMS unit arrives on scene.
7:10am: One more push and our beautiful baby boy with the surfer blond hair is born in the comfort (albeit, unplanned comfort) of our own home.
I held our baby only briefly before I had to hand him over to EMS for safe transport. Once we arrived at the hospital, I was finally able to snuggle (and latch!) my baby. I knew breastfeeding a baby with Down syndrome could be challenging but I also knew it was possible so it was important to me that he be introduced to the breast right away. He was headed to the NICU and I did not want to miss my window of opportunity. While he did take my breast in his mouth and manage to suck, he quickly fell off; almost as though he didn’t know what to do with it. Our time together came to an abrupt end as I watched my baby being whisked away, headed straight for the NICU for who knew how long.
Teaching Gage to breastfeed was a labour of love. It wasn’t until Gage was three days old that I was given the okay to attempt breastfeeding again. And even then, it was to be a quick attempt so as not to tire him and to ensure his tiny body was ready to take on the task of digesting food. Up until then, he hadn’t been fed at all. I had been pumping since his birth; my milk had come in and I was excited to latch him. But, there were tubes and wires and constant beeping machines to contend with and I was nervous. I managed to settle in and latch but again, he let go after only a couple of sucks. Our breastfeeding attempts had to be coupled with tube feedings and eventually, bottle feedings of pumped breastmilk because he just was not latching for long enough. I tried to be there for as many feedings as possible so I could latch him for each feed. He still wasn’t responding well, and we’d ultimately end up relying on the tube or the bottle. All the tube and bottle feeding was stressing me out. I wanted to nurse him and I was afraid the longer he tube/bottle fed for, the more my dream of breastfeeding would slip away.
One day, the nurse on duty suggested I try a nipple shield. At this point, I was willing to try anything. It was awkward at first but we were able to establish a strong enough latch to qualify as a feed. No need to follow up with the tube or the bottle. Hallelujah!! I was given the okay to breastfeed him three times a day. It was important to avoid overexertion and so, we alternated between breastfeeding and bottle feeding. By the time Gage was discharged from the NICU at eight days, we were successfully breastfeeding with a nipple shield and down to just three bottles per day. By two weeks old, Gage was exclusively breastfed without bottles. By three weeks, we lost the nipple shield. At three months old, Gage rejected the bottle altogether and continues to do so today. He loves mama’s milk! It was late spring when I finally realized we had reached a happy place in our breastfeeding journey. I was touring the zoo with my children, Ellie, was then a little over two, and Gage, who was four months. Ellie was in no mood to sit idly on a bench while Gage embarked on one of his marathon nursing sessions. So, in the sling he went. I latched him and he happily nursed while we continued with our tour. I remember breathing in the sweet smell of success in that moment. With plenty of pumping, but most of all, commitment, patience and perseverance, we had established breastfeeding. Gage was a pro.
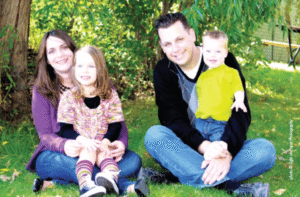
Breastfeeding was only the beginning of things Gage would learn. At 15 months old, he continues to hit those milestones and every single one of them is celebrated! He is a happy and healthy little boy who loves to charm people with his smile, squeal with delight at the sight of his big sister and, of course get into everything he shouldn’t be getting into. Remember those fears of him not being able to communicate or play with his sister or go fishing? What a ridiculous thing to ever think he couldn’t do those things! Gage proves to me every single day that he will do all of that and more.
People often ask if I would engage in prenatal testing again. While I thoroughly enjoyed being prepared, I now have to ask myself, if it doesn’t change our plans to bring a baby into the world unconditionally, is it worth the risk? Probably not. I struggle with the amount of misinformation, or complete lack thereof, available to couples. My hope and dream is that prenatal testing be preceded by mandatory information sessions led by medical professionals in order to receive accurate, balanced and unbiased information so that couples can make informed decisions both prior to and immediately after a prenatal diagnosis. It is natural to feel uncertainty and to fear what we don’t know. But, as someone who once feared but now knows, I can tell you Down syndrome is not to be feared. Down syndrome is such a tiny part of our lives; it’s what Gage has, not who he is.
I am also often asked whether I would plan a natural birth in the future. I never like to answer this definitively. I certainly desire for things to go as naturally as possible, but each birth experience is unique and brings about its own set of circumstances. I make decisions based on what is happening in the moment. But, I will say, having had both a hospital birth and an unplanned natural home birth, that my recovery and birth experience were far better with the latter. I can only imagine the interventions that would have taken place had Gage been born in the hospital, especially with the added concern of his heart condition. I am thankful he came into the world as he did and grateful for those who were there to assist with his birth. Who knew a firefighter could make a really great midwife?
When I think back to those images of what I thought my family would be like, I hadn’t imagined this. It’s more than I ever could have imagined. The love you have for your child from that very moment of conception is bar none. It will carry you through whatever it is you need to be carried through. I know our family is all the richer because of Gage. Being the parent of a child with special needs opens you up to a whole new perspective and makes you intrinsically want to be a better being; to dig deep and find your voice; to teach others compassion and acceptance. What an amazing gift he has brought to this world. At the tender age of 21 months, he has already taught so many.